Technological medical advancements have shifted an array of procedures previously rendered in inpatient hospitals to ambulatory surgical centers (ASCs). For example, same-day procedures (e.g., cataracts surgery) that do not require an overnight hospital stay and musculoskeletal procedures, such as arthroscopy, are commonly performed at ASCs.
Because they operate independently of brick-and-mortar hospital facilities, ASCs are considered "off site." Compared to procedures rendered in hospital outpatient departments, ASC's receive lower reimbursement. For low-risk procedures, ASCs may be a cost-efficient site of care. Recent market analysis found that procedures at ASCs have grown over time and now account for half of all outpatient surgeries.
In this brief, we compare employer-sponsored insurance (ESI) ASC reimbursement amounts for a subset of procedures to Medicare fee-for-service (FFS) payment for the same procedures. We find that, on average, ESI pays two times more than Medicare FFS for procedures provided at ASCs. If ESI reimbursed at Medicare average rates, spending would have been nearly $9 billion lower in 2021.
We limited this analysis to a basket of procedures approved by the Centers for Medicare and Medicaid Services (CMS) to be rendered and reimbursed at ASCs. Specifically, we limited our surgical procedure basket to procedures that: 1) were listed under the CMS ASC Covered Procedures List, and 2) were found in both ESI and Medicare FFS claims data with large volume in 2021. We analyzed the total reimbursed amounts (in other words, the total price for a procedure as observed in eligible submitted claims). We applied the same methodology as our previous brief comparing commercial and Medicare outpatient prices.
On average, ESI pays two times more than Medicare FFS for procedures rendered in ASCs in 2021
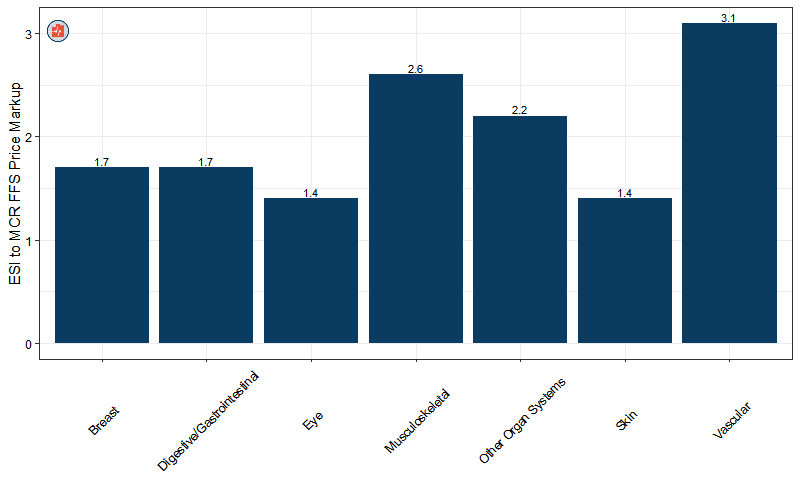
Figure 1: ESI to Medicare FFS reimbursement ratio for procedures in ASC setting
Figure 1 displays the ratio of ESI reimbursement to Medicare FFS reimbursement. For example, ESI reimbursement for vascular procedures were 3.1 times higher than the Medicare FFS payment rates. At the same time, ESI reimbursement for skin procedures were 1.4 times higher than Medicare FFS payment rates.
The vast majority of (76%) of ASC procedures studied have ESI payments that are greater than the corresponding median Medicare reimbursed amounts.
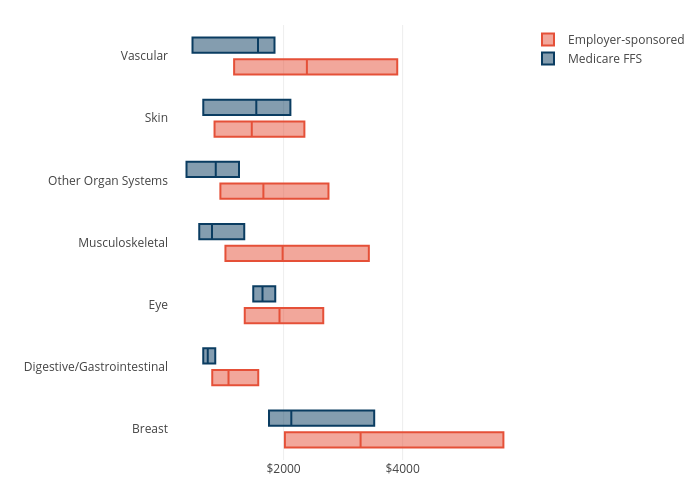
Figure 2: Reimbursement amount variation by type of procedures and payer
For each procedure category, there is variation in ESI and Medicare ASC payment amounts. Figure 2 shows the 25th, 50th, and 75th percentile total reimbursed amount by type of procedure for both ESI and Medicare in 2021. Generally, Medicare FFS reimbursement amounts have less variation than ESI amounts. For example, ESI payment for musculoskeletal procedures ranges from $1,023 at the 25th percentile to $3,432 at the 75th percentile in 2021, with a median payment of $1,984. Medicare FFS payments for musculoskeletal procedures, in contrast, range from a 25th percentile of $583 to a 75th percentile of $1,862, with a median payment of $798.
Greater variation among ESI payment rates is to be expected because they are the result of negotiations between payers and providers. Medicare FFS payments, on the other hand, are set administratively, so there is less opportunity for rates to differ.
For nearly all procedures, ESI reimbursement amounts were higher than Medicare FFS at the 25th, 50th, and 75th percentiles. Skin procedures were an exception. Although the 25th percentile ESI reimbursement and the 75th percentile ESI reimbursement were higher than Medicare, the median ESI ASC payment amount for skin procedures was lower ($1,465 for ESI compared to $1,541 for Medicare). Additionally, the variation in payment rates is similar between ESI and Medicare for skin procedures, unlike the other procedure categories.
Payment Rates for Procedures rendered at ASCs lower than the same procedures provided in Hospital Outpatient Departments
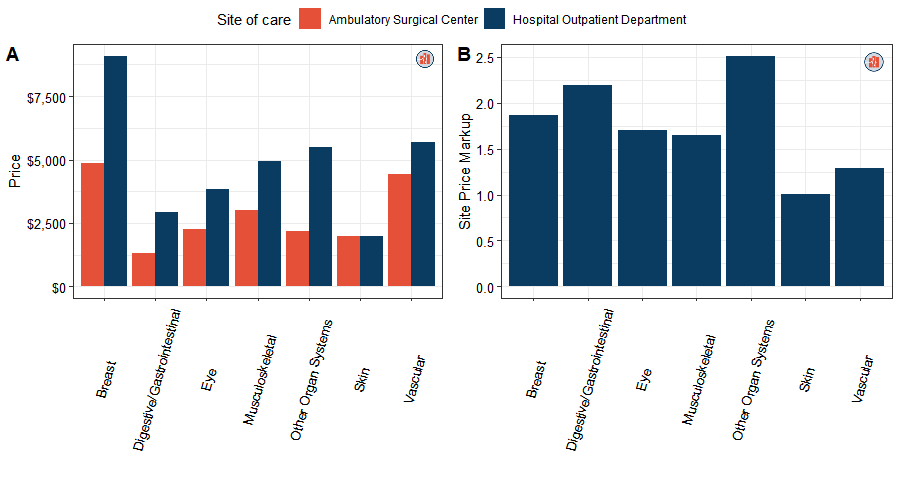
Figure 3: ESI reimbursement amounts between ambulatory surgical center and hospital outpatient
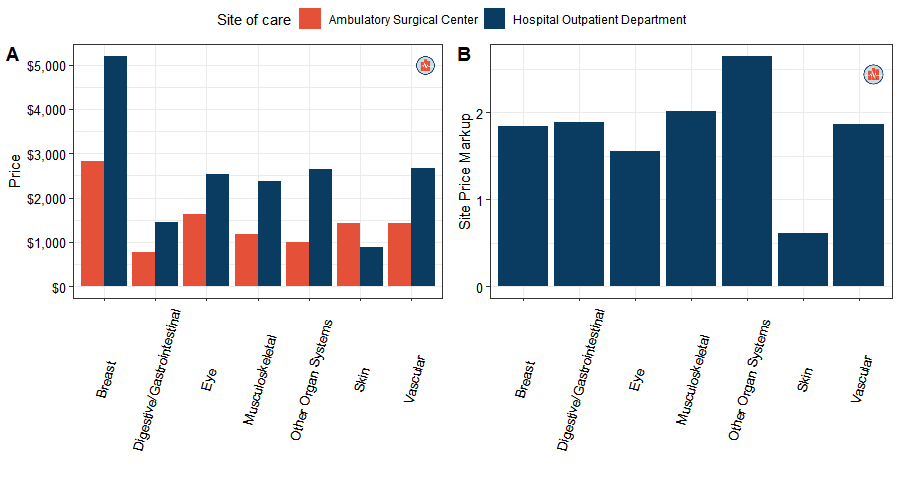
Figure 4: Medicare FFS reimbursement amounts between ambulatory surgical center and hospital outpatient
Our data also show that prices for procedures in ASCs are lower than the same procedure performed in hospital outpatient departments. This pattern is expected in light of higher overhead costs at hospital outpatient departments and is observed both in ESI and Medicare FFS (Figures 3 and 4). The reimbursed amounts for procedures performed at hospital outpatient departments are approximately 1.8 times higher, on average, for both payers (Figures 3B and Figures 4B). The difference was smallest for skin procedures, which indicates similar reimbursement amounts hospital outpatient departments and ASCs.
Most procedures are still primarily performed in hospital outpatient department for both insured populations.
Of the 453 eligible ASC procedures in our study, most are performed in hospital outpatient departments (Figure 5). This finding was true for both ESI and Medicare and may suggest that a substantial number of patients requiring outpatient procedures have factors or circumstances that put them at higher risk of complications or otherwise make the outpatient department a more appropriate site of care. . With the exception of eye and musculoskeletal procedures, hospital outpatient departments account for a higher share of all types of procedures for both payers. Eye procedures, primarily for cataracts removal, deviate from this trend; most procedures in this category are rendered in ASCs in both ESI and Medicare FFS populations.
Figure 5: Site of care proportion by types of procedures and payers
Simulated savings suggest that ESI could save about $9B if ASC procedures were reimbursed at average Medicare rates.
To illustrate the effect of the difference between ESI and Medicare reimbursement, we estimate the potential savings if ESI payment rates equaled average Medicare rates. If ASC procedures among ESI enrollees were reimbursed at Medicare FFS ASC rates, ESI payers could save approximately $9.3B in one calendar year. The majority of the savings are the result of savings from musculoskeletal ($3.8B) and gastrointestinal procedures ($2.8B).
Figure 6: Estimated total ESI savings if all procedures are performed in ambulatory surgical centers
Considerations for Policymakers and Future Research Directions
In this brief, we found that reimbursement amounts in ASCs are lower than HOPDs for both Medicare FFS and ESI payers. Consistent with previous research, Medicare FFS reimbursement amounts are lower than ESI reimbursement amounts at both sites of care.
Although procedures provided in ASCs can be cost-effective compared to procedures rendered in HOPDs, there are some patients, particularly those with baseline higher risk of complications, where procedures in HOPDs are more appropriate. In this brief, we do not specifically account for patient health characteristics nor does this brief draw any conclusions on clinical appropriateness of site of care.
As more procedures shift to ASCs, it is important to track use, cost, and spending for services provided in that site of care. Recent evidence has shown that ASCs have increasingly become the subject of private equity acquisitions in recent years, likely in part because they have lower fixed operating costs than hospital outpatient departments. It will be important to understand the impact of private equity investment on cost and quality.
Additionally, limited information on ASCs' operational costs complicates policymakers' and researchers' efforts to understand the potential for ASCs to achieve efficiency and provide value. MedPAC's has recommended that the HHS Secretary require ASCs to report cost data. Additional information on ASC use, costs, and spending will add to public and private policymakers' understanding of the potential for these settings to improve value in the US health care system.
Methods
We used 2021 outpatient and carrier claims data from both HCCI employer-sponsored insurance and Medicare fee-for-service. We limited our data to ASC claims (defined as place of service set to 24 in CMS-1500 claim form or type of bill 83x in UB-4 facility claim form, where the claim was for the primary payer. Additionally, we included payments to Critical Access Hospitals (exclusive of physician payments) in our payment rate calculations. To ensure comparability between both Medicare FFS and ESI claims data, we removed the following claims from both datasets: home health, skilled-nursing facility, hospice, inpatient claims, Federal Qualified Health Clinics, dialysis, ambulance, durable medical equipment, and therapy. These services are paid under substantively different payment rules, which limits our ability to meaningfully compare prices between Medicare and ESI. We further limited our ESI claims data to final adjudicated claims. Medicare claims were limited to those with allowed amounts greater than $0; Medicare data include outlier payments in average rate calculations, but no other adjustments based on case mix were made.
We leveraged the 2021 Ambulatory Surgical Center (ASC) Payment from Center for Medicare and Medicaid Services (CMS) to evaluate our 2021 ESI ASC claims groupings. All items and services paid under the Hospital Outpatient Prospective Payment System (OPPS) are assigned to APC payment groups that are similar in clinical and resource use. For this analysis we aggregated payments for services following ASC payment logic on ASC claims. We limited our analysis of ESI and Medicare reimbursement amounts to ASC procedures found in both ESI (>1500 claims) and Medicare claims. ESI use and allowed amounts were weighted using ESI weights to develop estimates that were representative of the national ESI population under 65 years old. ESI weights were calculated using the American Community Survey (ACS) 2021 5-year estimates Public Use Microdata Sample (PUMS).