In 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children's Hospital Association, declared a National State of Emergency in Children's Mental Health associated with the COVID-19 pandemic, including the loss of caregivers, school closures, social isolation, and gaps in health care (see citations below). Understanding the effect of the COVID-19 pandemic on children's mental health is critical to ameliorating that impact and preparing for future pandemics.
News reports as well as data from the Centers for Disease Control and Prevention and others have highlighted children's use of the emergency room (ER) for mental health reasons as a particularly concerning trend during the pandemic. In this brief, we examine this issue among children with employer sponsored health insurance (ESI) using HCCI's claims dataset. We find that, even as overall ER use decreased in 2020, the first year of the COVID-19 pandemic, the share of children's ER visits that were for mental health needs increased, especially among adolescents. Over the same period, the share of ER visits that were for mental health needs declined among adults.
The increase in the share of children's ER visits for mental health needs in the first year of the pandemic is just a small component of how the pandemic has affected children in the U.S. While these data are far from the whole picture of children's mental health care needs and services, use of the ER for mental health needs is likely a signal of more widespread need in this population, especially in this and future crises.
The Share of Children's Emergency Room Visits for Mental Health Rose in April 2020 and Remained High for the Rest of the Year
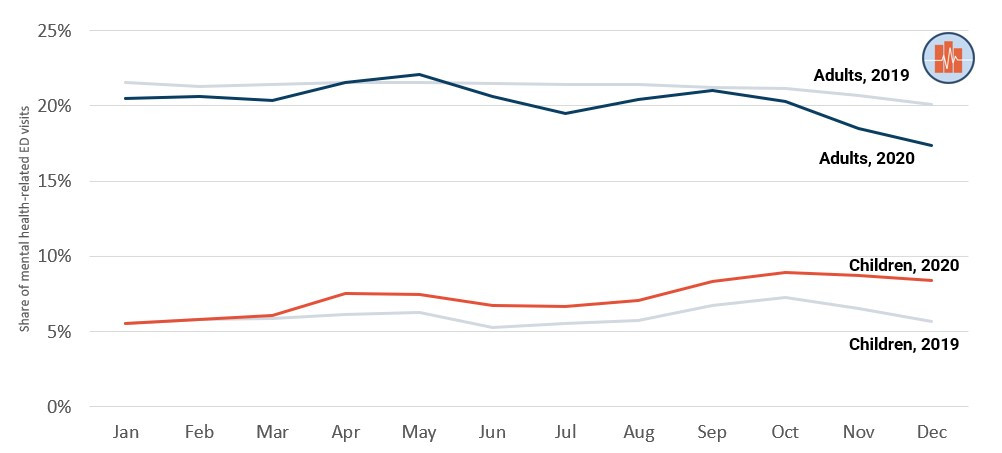
As shown in Figure 1, the share of ER visits for mental health needs among children with ESI increased in 2020 relative to 2019 (see Methodology for details on how we identified mental health-related ER visits). This increase began in April of 2020, in the early stages of the COVID-19 pandemic. In January-March 2020, the percent of ER visits for mental health needs was similar to the same time period in 2019. In April 2020, however, the share of ER visits for mental health needs increased to 7.6% among children, 1.4 percentage points higher than the rate in April 2019 (6.2%). The share of ER visits for mental health needs remained higher throughout the rest of 2020 compared to 2019, with the largest difference in December (8.4% of visits in 2020 compared to 5.7% of visits in 2019).
In contrast, the share of ER visits for mental health needs among adults was similar or lower in 2020 compared to 2019. The shares in 2018 were similar to 2019 (see the Downloadable Data accompanying this brief).
Figure 1. The Percent of ER Visits for Mental Health Increased in 2020 Compared to 2019 Among Children, but Decreased for Adults
Among both children and adults, there was a substantial decline in the use of the ER overall in 2020, as shown in previous HCCI and other work (as well as in the Downloadable Data available with this brief). Accordingly, the higher share of children's ER visits for mental health needs was driven by a smaller decline in the number of ER visits for mental health compared to ER visits for other reasons. That the number of mental health visits did not decline as much as other types of visits indicates that many children continued to need and use these services even as overall use declined.
Growth in the Share of Children's ER Visits for Mental Health Needs was Driven by Adolescents
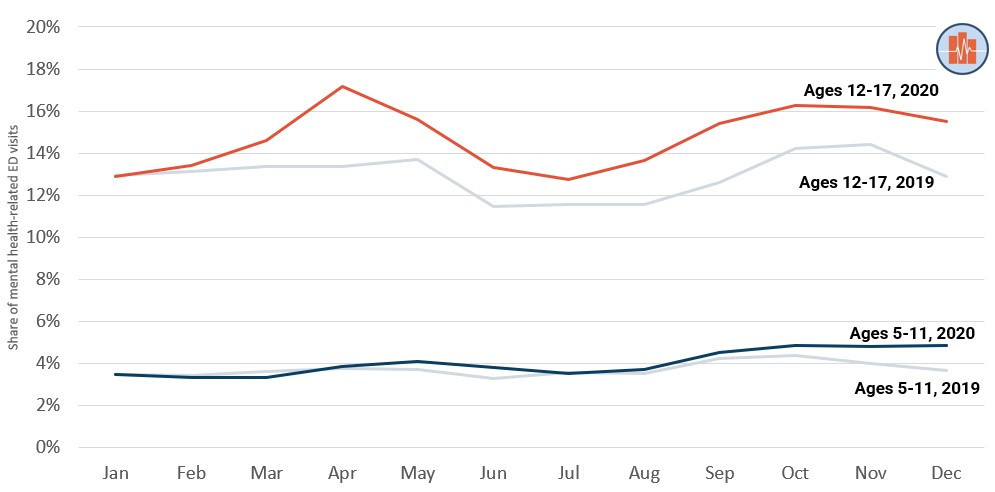
In 2020, there was a relatively sharp increase in the percent of visits for mental health needs among adolescents (ages 12-17), as shown in Figure 2. In April 2020, just over 17% of visits among adolescents were for mental health needs compared to about 13% of visits in April 2019. The share remained higher for the rest of 2020, with especially large differences between 2020 and 2019 in September (15% of visits in 2020 compared to 13% in 2019) and December (16% of visits compared to 13%).
In contrast, the shares of ER visits for mental health needs among children ages 5-11 were similar in 2020 and 2019, with only a slight increase in December (5% of ER visits were for mental health needs in December 2020 compared to 4% of visits in 2019). The Downloadable Data available with this brief includes data on children ages 1-4; children in this youngest age group had under 1% of ER visits for mental health needs in all years of our data.
Figure 2. Adolescents Experienced a Greater Increase in the Share of ER Visits for Mental Health than other Children in 2020 Relative to 2019
Continued Use of the ER for Mental Health Care among Children in 2020 Motives Further Policy and Health Care System Action to Ensure Children's Needs are Met
In 2020, the first year of pandemic, the share of ER visits for mental health needs rose among children with ESI, even as overall ER use fell. This rise was driven by an increase in the share of ER visits for mental health among adolescents. Our findings reflect the stresses on children during the pandemic, including losing caregivers and access to school support systems.
Preliminary analyses also suggest that adolescents stayed slightly longer in the ER for mental health needs in 2020 compared to earlier years, though the reasons for mental health visits (e.g., the share due to behavioral disorders, anxiety) appear to have remained stable over time. We also observed a slight increase in the percent of children with a mental health-related ER visit who had a repeat visit to the ER within a month of discharge. These trends call for further assessment and monitoring as additional data become available.
Ensuring that children receive appropriate mental health services is critical for their well-being, including emotional and physical health and educational success. Children's mental health also influences parents' well-being and ability to work and has ripple effects across the health care system. A deeper understanding of how the pandemic impacted mental health will allow policymakers and practitioners to structure solutions for both crisis and non-crisis times.
Methods
We identified outpatient claims for emergency room visits using CPT codes from 99281 to 99285 or revenue center code values of 0450-0459. Cases where multiple ER E&M codes were billed to the same patient on the same day counted as one visit. Presence of a MH diagnosis was identified by the occurrence of any of the following International Classification of Diseases Version 10 (ICD-1O) codes in any diagnostic field: F01-F99.x.
The average proportion of ED visits were calculated by dividing average number of ED visits for mental health diagnosis in a given month and year with the average total number of ED visits within the same month and year.
We excluded visits that have less and equal to $1 total spending. We defined as the difference of year of birth and outpatient visit date, and we excluded children younger than 1 year old. We finally excluded patients with no sex information, or with multiple sex or year of birth, or CBSA within a month. We included claims where ESI flag is equal to one, products within EPO, HMO, POS, PPO, claims were paid as primary coverage, and claims with mental health coverage.