All HCCI Reports
Health Affairs: Surprise Bills, Benchmarks, And The Problem Of Indexation
HCCI data was cited in a Health Affairs blog article on surprise billing.
From the Article:
"Over the past year, the congressional debate over surprise billing has converged on two policy options to resolve out-of-network payments—1) a simple benchmark, in which a health plan pays out-of-network providers the median rate agreed with local in-network providers in the same specialty, or 2) a similar benchmark combined with optional arbitration if the provider or payer objects to that default amount. These reforms would dent staffing company and hospital revenues by only 0.75 percent to 1.00 percent over the next 10 years—while aggregate hospital and physician revenues rise by more than 60 percent, or $1.6 trillion—yet, the legislation has sparked a furious lobbying campaign to perpetuate the status quo. Meanwhile, the Sturm und Drang over arbitration has eclipsed discussion of other policy details, some of which could create pernicious long-term distortions in a market already mired in dysfunction..."
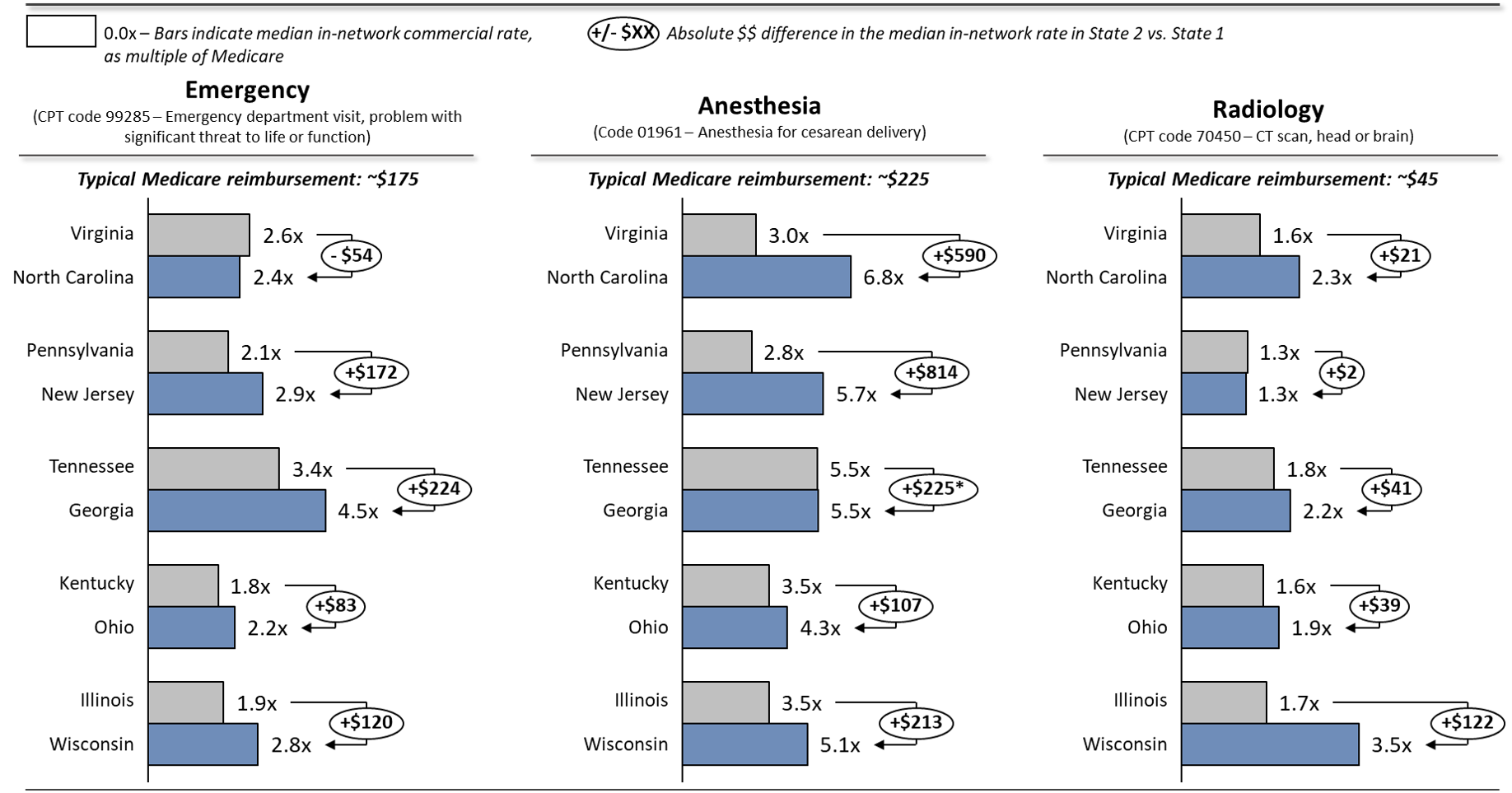
"Source: Authors' analysis of Health Care Cost Institute (HCCI) 2017 data based on Hargraves J, Biniek J. Comparing commercial and Medicare rates for select anesthesia, emergency room, and radiology services by state. Washington (DC): HCCI; 2019 Jul 23. Notes: Medicare reimbursement varies by market, given the geographic practice cost indices incorporated into the Medicare payment formula. "Typical" amounts shown here reflect the approximate unweighted national average in 2017. *The median rate for code 01961 in both Tennessee and Georgia is approximately 5.5x Medicare, but the average Medicare reimbursement differs by $41, which results in the absolute dollar difference between the median commercial reimbursement in these two states."
When you subscribe to the blog, we will send you an e-mail when there are new updates on the site so you wouldn't miss them.